-
Climate Change: Influence on the Spread of Lyme Disease
By Roberta Attanasio Blacklegged ticks feed on blood — they attach to the skin of humans and many animals and, slowly, suck for several days. To get there, they patiently wait on the tip of grasses and shrubs using their lower legs to hold on, until a human or an animal passes by. Ticks can’t jump or fly, so they keep their upper pair of legs outstretched, ready to climb aboard. Once there, they insert their feeding tube into the skin and start to suck the blood — this is how they become infected by or transmit Borrelia burgdorferi, the micro-organism that causes Lyme disease. Lyme disease is one of the most common infectious diseases in…
-
Tuberculosis in China: A Success Story for a Global Problem
By Roberta Attanasio Sometimes called “The Silent Killer”, tuberculosis, or TB for short, is a huge worldwide public health problem — according to the World Health Organization (WHO), one-third of the human population is infected with Mycobacterium tuberculosis, the micro-organism that causes the disease. In 2012, an estimated 8.6 million people developed TB and 1.3 million died from it. The number of TB deaths is unacceptably large, given that most are preventable — indeed, a cure for TB, consisting of a six-month course of drugs, has been available for more than 50 years. If treatment is incomplete, TB can come back, often in a form resistant to treatment. Years ago, the WHO developed a strategy known…
-
A New Kind of Global Die-Off: Bananas Hit by Rapidly Spreading Diseases
By Roberta Attanasio The world loves bananas. Actually, the world loves the Cavendish bananas, mostly because it is (almost) the only variety commercially available worldwide. The entire global banana industry relies on this seedless and, therefore, sterile variety made of bananas all essentially identical to each other — and equally susceptible to infection by the same harmful microbes, which can spread very easily across plantations around the world. This is not a hypothetical scenario — instead, it’s happening as we speak. Two species of fungi are threatening the world supply of the Cavendish bananas. One is Mycosphaerella fijiensis, a fungus that causes a disease dubbed Black Sigatoka, also known as…
-
Sex Differences in the Immune Response to Vaccines
By Roberta Attanasio Women and men respond differently to infectious microbes and vaccines – it is said, indeed, that the immune system of women is stronger than the immune system of men. Stronger or weaker, one thing is certain – men and women are not the same in terms of immune response. A few years ago, the journal Lancet Infectious Diseases published “ The Xs and Y of immune responses to viral vaccines” – a comprehensive article that clearly shows how the biological differences between sexes influence the immune response to vaccines, as for example the influenza, yellow fever and hepatitis vaccines. There are not many published studies on the…
-
Wasting Syndrome and Starfish Die-Off
By Roberta Attanasio Up and down the U.S. and Canada Pacific coastlines, starfish are disappearing, dying by the millions of a mysterious disease that makes them “turn into goo.” The disease — starfish wasting syndrome — initially causes white lesions that lead to death of body tissue. Eventually, the arms twist and tear off — and they do not regenerate (healthy starfish may shed their arms, but then new ones are formed in a relatively short time). At the end, the entire body of the wasting starfish disintegrates. The wasting syndrome affects about a dozen starfish species, but has been noticed mostly in sunflower starfish (Pycnopodia helianthoides) and ochre stars (Pisaster ochraceus). Starfish…
-
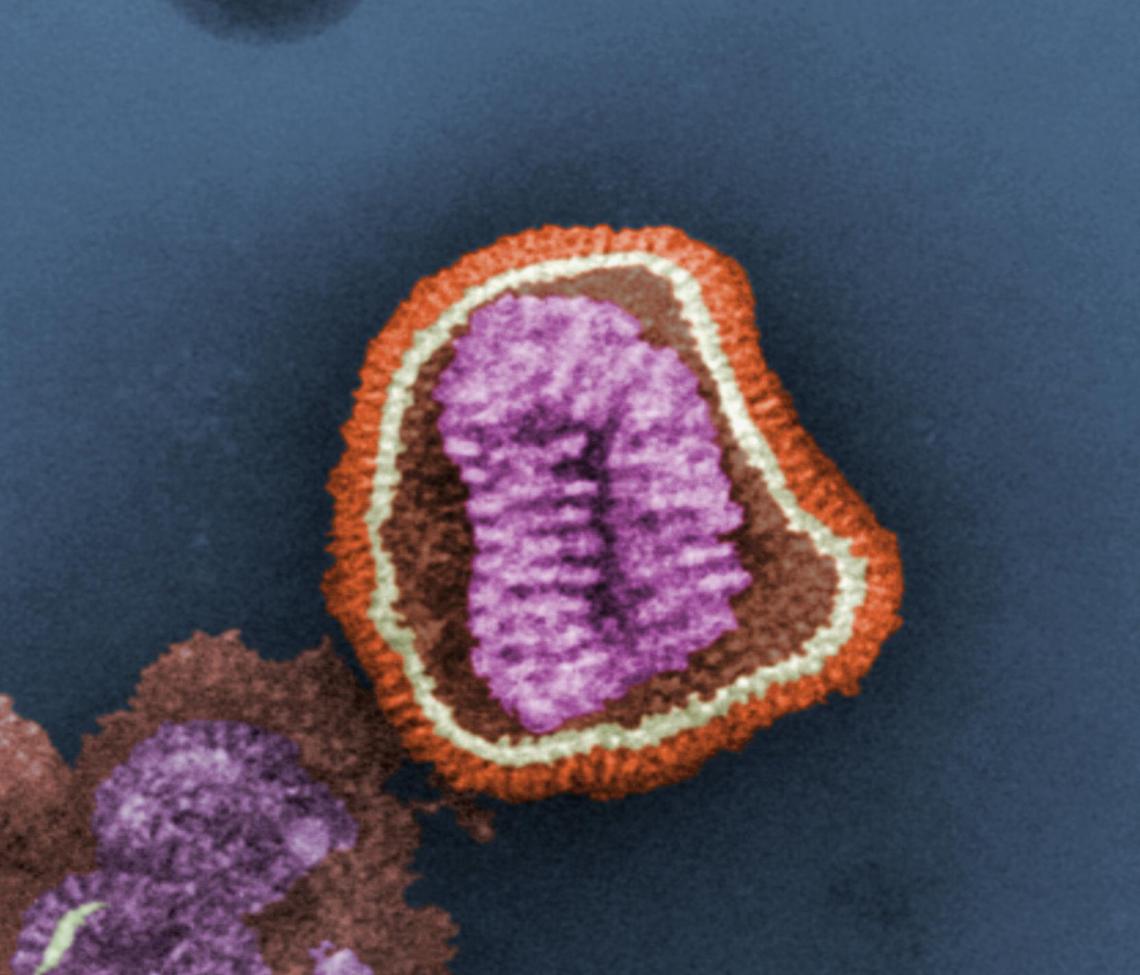
H7N9 Influenza Virus: Ethnicity and Protection from Infection
By Roberta Attanasio In March 2013, a new flu virus — the H7N9 — was identified in China. By early May, before retreating and disappearing, it had infected 131 people and killed 26 of them. However, less than two weeks ago (January 17), the New York Times reported that “China is disclosing a steadily growing number of cases of H7N9 bird flu, including four more cases announced on Friday, reviving concerns among health experts that the disease may be spreading and could pose a further threat as the world’s largest annual human migration begins ahead of Chinese New Year.” The H7N9 virus is a “reassortant” — it includes combined elements from three…
-
A Toxoplasma’s Journey: From Cats to Sea Otters
By Roberta Attanasio Toxoplasma gondii is a single-celled parasite that infects most warm blooded animals. In 2012, it landed in the news because of its ability to hijack the arousal circuitry of rats — the parasite activates a part of the brain normally engaged in sexual attraction. Rats infected with it are not afraid to approach cats and behave as they would in the presence of a sexually receptive female rat. What happens next? The cat easily catches and eats the infected rat and, in doing so, also catches the parasite — the parasite is happy as it reproduces sexually only in cats. The parasite’s oocysts — sometimes called “eggs”…
-
Arsenic Contamination of Drinking Water in India Impairs Kala-Azar Treatment
By Roberta Attanasio Visceral leishmaniasis, known in India as kala-azar or black fever, is a parasitic disease that kills an estimated 500,000 people a year, 90 percent of them in India, Nepal, Bangladesh, Brazil and Sudan. In India, the disease is endemic in the northeastern Indian State of Bihar – the epicenter of kala-azar in the region – and in Jharkhand, Uttar Pradesh and West Bengal. It manifests with irregular bouts of fever, substantial weight loss, swelling of the spleen and liver, and anemia. Left untreated, kala-azar is almost always fatal, especially in children, According to the World Health Organization (WHO), “Leishmaniasis is a poverty-related disease. It affects the poorest…
-
The Great Global Die-Off: Frogs and Lymphocytes
By Roberta Attanasio Frogs and other amphibians – salamanders and caecilians – have been declining worldwide during the past few decades at an alarming rate. According to a June 2012 assessment by the International Union for the Conservation of Nature and Natural Resources (IUCN), about 41 percent of amphibian species are at risk of extinction, and some are already extinct. Like many other inhabitants of our planet, amphibians have been hit hard by climate change and habitat loss – and not only. Amphibians have also been decimated by the spread of chytridiomycosis, which is defined by the IUCN as the single most devastating infectious disease of vertebrate animals. In a…
-
Arsenic in Drinking Water: Increased Risk of Respiratory Infections and Lung Damage Following Fetal Exposure
By Roberta Attanasio Odorless and tasteless, arsenic lurks everywhere – in rice and in chicken breasts, in apple juice and in drinking water. It’s all around, but not in amounts sufficient to cause acute (short-term) poisoning. On the other hand, chronic (long-term) exposure to lower arsenic doses occurs way too often, and may lead to cardiovascular disease, diabetes, cancers and other human disorders. Contamination of drinking water by arsenic is a global health threat. Presence of arsenic in groundwater is largely the result of minerals dissolving from weathered rocks and soils. In addition, arsenic enters the drinking water supply because of runoff from orchards, electronics production waste or other industrial…